ORIGNAL ARTICLE | https://doi.org/10.5005/jp-journals-10049-0092 |
Comparison of Ultrasound-guided vs Blind Transversus Abdominis Plane Block in Gynecological Abdominal Surgeries for Postoperative Analgesia in Tertiary Care Center: A Randomized Prospective Single-blind Study
1Department of Anesthesia, Seth GS Medical College, Mumbai, Maharashtra, India
2Department of Anaesthesiology, Dr DY Patil Medical College and Research Institute, Pune, Maharashtra, India
3Department of Anesthesia, King Edward Memorial Hospital, Mumbai, Maharashtra, India
4Department of Anaesthesiology, Seth GS Medical College, Mumbai, Maharashtra, India
Corresponding Author: Harsha Narkhede, Department of Anaesthesiology, Dr DY Patil Medical College and Research Institute, Pune, Maharashtra, India, Phone: +91 9820120440, e-mail: hhnarkhede@gmail.com
How to cite this article Shrikanta Oak, Narkhede H, Poduval D, et al. Comparison of Ultrasound-guided vs Blind Transversus Abdominis Plane Block in Gynecological Abdominal Surgeries for Postoperative Analgesia in Tertiary Care Center: A Randomized Prospective Single-blind Study. Res Inno in Anesth 2021;6(1):5–10.
Source of support: Nil
Conflict of interest: None
ABSTRACT
Background and aims: The transversus abdominis plane (TAP) block is a recently described approach which blocks the nerves of the anterior abdominal wall. We compared the duration of analgesia and efficacy of ultrasound-guided vs conventional block on immediate postoperative pain in patients undergoing gynecological abdominal surgeries.
Materials and methods: Eighty-two patients undergoing gynecological abdominal surgeries under spinal anesthesia were randomized to undergo ultrasound-guided (n = 41) vs anatomical landmark-guided TAP block (n = 41). The pain severity using the visual analog scale (VAS) score at rest and on movement were noted at various time intervals up to 24 hours. We compared the total duration of analgesia (TDA) and the total consumption of analgesics (TCA) in both groups. SPSS version 21 was used. Demographic data were analyzed using the Student’s t-test and other parameters using paired t-test.
Results: Mean VAS scores both at rest and on movement were significantly higher in the anatomical landmark-guided TAP block in the first 8 hours postoperatively. The TDA was prolonged significantly (18.88 ± 6.18 hours) and TCA was less (0.95 ± 0.67 g) in the ultrasound group as compared to the other group with TDA of 8.38 ± 2.58 hours and TCA of 2.54 ± 0.71 g.
Conclusion: Ultrasound-guided TAP block provided a significantly longer duration of analgesia as compared to the anatomical landmark-guided TAP block and a significant decrease in consumption of rescue analgesics.
Keywords: Postoperative pain, Transversus abdominal plane block, Visual analog scale..
INTRODUCTION
Nowadays the concept of fast track surgery has developed with the aim of enhanced recovery with minimal complications and reduced hospitalization.1 Opioid-sparing multimodal analgesia (like neuraxial block, regional block, nonsteroidal anti-inflammatory drugs (NSAIDs), paracetamol) is an essential part of enhanced recovery after surgery. Epidural analgesia was the standard method for postoperative pain management in abdominal surgeries till now but recent literature does not support the same.2 Regional nerve block especially useful in patients with coagulopathy, poor cardiopulmonary reserve, and in hemodynamically unstable patients where epidural technique would be contraindicated. Only NSAIDs and paracetamol are not sufficient but are the supplements to the other modes of analgesia.
Transversus abdominis plane (TAP) block has been described as an effective technique as a part of multimodal analgesia to reduce postoperative pain and opioid consumption after lower abdominal surgeries.3 Though Carney et al.4 had observed the analgesic benefits of transversus abdominis block in total abdominal hysterectomy (TAH) by anatomical landmark method and Atim et al.5 observed the same with ultrasound, there is no study on the comparison about efficacy and duration of analgesia of ultrasound-guided vs conventional transversus abdominis block in patients undergoing gynecological abdominal surgeries.
We thus conducted a randomized prospective single-blind study to compare the duration of analgesia and efficacy of ultrasound-guided vs conventional transversus abdominis block on postoperative pain relief up to 24 hours, hypothesizing that conventional TAP block will also demonstrate similar efficacy of pain relief which would be of benefit in centers where USG is not available.
MATERIALS AND METHODS
After Institutional Ethical Committee approval, CTRI registration (CTRI/2018/05/013811) and written informed consent, 82 (41 in each group) adult female patients of ASA physical status I to II undergoing elective abdominal gynecological surgeries (TAH and exploration for ovarian cystectomy, postpartum tubal ligation) under spinal anesthesia were recruited for the study for the period of 6 months. This study was designed to be a randomized prospective single-blind study. Exclusion criteria were: refusal by the patient, morbid obesity, surgical scar or distorted anatomy at the site of injection, redo surgeries, known allergy to local anesthetics. Forty-one patients in each group would be needed after assuming the probability of alpha error as 1% and the power of the study as 80%, confidence interval of 99%. Patients were allocated randomly by sealed envelopes, according to a computer-generated sequence of random numbers, to undergo ultrasound-guided (Group U) vs anatomical landmark-guided TAP block (Group A).
The primary objective of the study was to compare the duration of postoperative analgesia in both groups. Secondary objectives were to compare the efficacy with respect to VAS score at various time intervals, 24-hour consumption of rescue analgesics, hemodynamic stability, and complications like hematoma, local anesthesia systemic toxicity, and visceral injury in both the groups. Written informed consent was signed by the patients who are willing to participate in the study.

On the day of operation, after confirming starvation status the patient was taken to operation theater and intravenous (i.v.) fluid started. Standard ASA monitoring was used for all patients. Heart rate (three-lead ECG), noninvasive arterial pressure, and oxygen saturation were continuously monitored perioperatively. All patients received routine subarachnoid block with 3.5 cm3 of injection bupivacaine heavy with 0.5 cm3 of injection fentanyl as additive with 25 G spinal needle under all aseptic precautions. Bilateral transversus abdominis block was given postoperatively as part of multimodal analgesia. Receding sensory and motor block was assessed by two-segment regression and ankle movement, respectively. All the blocks were performed postoperatively after confirmation of motor block regression (by observing ankle movement) by a senior anesthesiologist having experience of >5 years in regional anesthesia.
USG-guided Tap Block (Group U)
Transversus abdominis plane block was performed under ultrasonographic guidance with a high-frequency linear probe (6–13 MHz) in the supine position.
The drug was given with 20 G Angiocath stylet, using the in-plane technique. The ultrasound probe was prepared in a sterile manner.
External oblique, internal oblique, and transverses abdominis muscles were visualized between the subcostal margin and iliac crest (Fig. 1A).
Once the tip of the needle was placed in a space between the internal oblique and transversus abdominis muscles, a test dose of 1–2 mL of saline 0.9% was given to visualize the needle tip location. A probe was adjusted continuously to visualize a bright hyperechoic shaft and tip (Fig. 1B).
When the needle tip was in the correct plane 20 cm3 of 0.25% injection bupivacaine, was administered on each side under direct USG guidance, after negative aspiration of blood.
The drug spread was visualized as an ellipsoid shape dark shadow forming between the aponeurosis of the internal oblique and the transversus abdominis muscles (Fig. 1B).
The total dose of bupivacaine was 2 mg/kg and the total volume was not >40 mL.
Anatomical Landmark-guided (Blind) Tap Block (Group A)
Blind TAP block was given with anatomical landmark method. 20 G Angiocath stylet was inserted in a lumbar triangle of petit (bounded by latissimus dorsi posteriorly, external oblique anteriorly, iliac crest inferiorly, and internal oblique muscle at the floor) above the highest point of the iliac crest in mid-axillary line in the supine position. This field block involves the injection of local anesthetic deposition between the internal oblique and transversus abdominis muscle. After confirmation of double loss of resistance technique and backflow with 1–2 mL of normal saline, 20 cm3 of 0.25% injection bupivacaine was administered with intermittent aspiration on both sides each.

Figs 1A and B: (A) Showing external oblique, internal oblique and transverses abdominis muscles; (B) Showing bright hyperechoic shaft and tip of needle and ellipsoid shape dark shadow was confirmed while injecting the drug between the aponeurosis of internal oblique and the transversus abdominis muscles
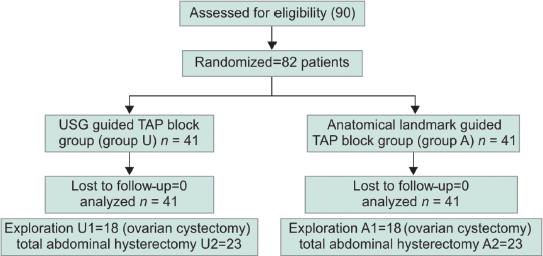
Flowchart 1: Consort flow diagram. PTL, postpartum tubal ligation
| Parameters | Group U (n = 41) | Group A (n = 41) | Significance |
|---|---|---|---|
| Age (years) | 37.49 ± 8.98 | 40.44 ± 11.62 | p > 0.05 |
| Weight (kg) | 56.78 ± 8.65 | 56.39 ± 9.34 | p > 0.05 |
| ASA (I and II) | 39/2 | 37/4 | p > 0.05 |
| Duration of surgery (min) | 124 | 122 | p > 0.05 |
| Duration of anesthesia (min) | 174 | 176 | p > 0.05 |
ASA: American Society of Anesthesiologists + values are expressed in terms of mean ± SD. (Duration of anesthesia was measured from the time of spinal anesthesia till two-segment regression of sensory level from T6 and ankle movement.)
The anesthesiologist who performed the block was not involved in postoperative data collection. Parameters like pain severity using a visual analog scale (VAS) score at rest and knee movement every 2, 4, 8, 12, 18, and 24 hours postoperatively, hemodynamic at 2, 4, and 8 hours postoperatively, and complications for 24 hours were assessed. Patients were instructed how to make use of a 10 mm VAS graded from 0 (no pain) to 10 (most severe pain) preoperatively.
Injection paracetamol 15 mg/kg was given intravenously as the first rescue analgesic in both the groups when VAS score >4. We decided to give injection diclofenac as a second rescue analgesic if pain relief was not achieved with paracetamol also noted consumption of injection paracetamol in 24 hours (Flowchart 1).
STATISTICAL ANALYSIS
Data were statistically described in terms of mean (±SD), frequencies (number of cases), and percentages when appropriate. Comparison of quantitative variables between the study groups was done using an unpaired t-test. For comparing categorical data, a Chi-square test was performed. An exact test was used instead when the expected frequency is <5. The confidence interval considered was 99%. A probability value (p value) <0.05 was considered statistically significant. All statistical calculations were done using computer programs Microsoft Excel 2013(Microsoft Corporation, NY, USA) and SPSS (Statistical Package for the social science, SPSS Inc., Chicago, IL, USA) version 21.

Fig. 2: Comparison of total duration of analgesia and total consumption of analgesia
RESULTS
Patients in both the groups were comparable in terms of demography, ASA status, total duration of anesthesia, and surgery; a summary of which has been shown in Table 1.
From the analysis of hemodynamic parameters in terms of pulse rate, systolic BP, and diastolic BP up to 2, 4, and 8 hours postoperatively, it was found that all of them were comparable and not statistically significant in both the groups.
Injection paracetamol 1 g was the first line analgesics and injection diclofenac was the second line analgesics. The total duration of analgesia (TDA) was noted in both the groups as the time from block till they received first rescue analgesics.
We found that the TDA and total consumption of analgesics (TCA) were statistically significant (p < 0.05) in both groups. The TDA was prolonged significantly in the USG-guided TAP block group (Group U) (18.88 ± 6.18 hours) as compared to the anatomical landmark-guided TAP block group (Group A) (8.38 ± 2.58 hours) (Fig. 2).

Fig. 3: Comparison of duration of analgesia and consumption of rescue analgesia in exploration cases

Fig. 4: Comparison of duration of analgesia and consumption of rescue analgesia in TAH case

Figs 5A and B: VAS score at rest (A) and movement (B)
We observed that total consumption of analgesia is less in surgical patients who underwent exploration (U1 and A1) cases in comparison with patients who underwent TAH (U2 and A2) cases. So, we did a further subgroup analysis and we found a statistically significant difference in TDA and total consumption of analgesics (TCA) in subgroups (Figs 3 and 4). In anatomical landmark-guided TAP block (Group A) requirement of injection paracetamol (total consumption of analgesics) was more than 2.54 ± 0.72 g in comparison with 0.95 ± 0.67 g in USG-guided TAP block (Group U) which was statistically significant. In both groups, patients did not require a second rescue analgesic at all. Patients of postpartum tubal ligation which were included in exploration cases did not require paracetamol for 24 hours.
Mean of VAS score both at rest and movement (knee flexion) was comparable and higher in anatomical landmark-guided TAP block group (Group A) than in USG-guided TAP block group (Group U) at 2, 4, and 8 hours postoperatively which was statistically significant. After 8 hours when the patient received injection paracetamol in the anatomical landmark-guided TAP block group (Group A). The mean of VAS was comparable in both the groups but not statistically significant (Fig. 5). None of the patients had any complications in both the groups which can be attributed to TAP block.
DISCUSSION
Epidural analgesia was the common pain relief technique for postoperative analgesia in the past for many surgical procedures. But now with more and more use of anticoagulants as prophylaxis and the advent of a concept of fast track recovery, the risk-benefit ratio for epidural analgesia is still a question. So less invasive techniques like nerve blocks with minimal complications are being considered.
Transversus abdominis block is a fascial plane block. It was introduced in anesthesia practice by Rafi in 2001 using the traditional landmark of a lumbar triangle of petit.6 This block requires a larger volume of local anesthetics to deposit it in-between the aponeurosis of the internal oblique and transversus abdominis. Transversus abdominis plane block innervates the nerves of the anterolateral abdominal wall including the parietal peritoneum. The analgesic effect of TAP block may last longer maybe because of the less vascular plane at that site as the absorption of local anesthetics into the circulation depends primarily on the vascularity of the site of deposition.7 The mean TDA was 18.67 hours in our study with ultrasound while Mankikar et al.8 found a mean duration of 9.53 hours after TAP block in cesarean patients. This duration can further be prolonged by additives like clonidine.9
Many studies have proved until now that the TAP block provided effective analgesia during the first 24 hours after surgeries of lower abdominal or pelvic surgical procedures3,4 in which they had included a limited number of patients for each surgical procedure and comparisons were performed with a control group receiving systemic analgesia.
Transversus abdominis plane block can be successfully given using the anatomical landmarks in the lumbar triangle of petit by the double loss of resistance technique and by confirmation of backflow. McDonnell et al.3 and Carney et al.4 found a decrease in the postoperative VAS score after the block was given by the anatomical landmark method in abdominal surgeries and TAH, respectively.
But when we perform the TAP block blindly, the drug can be incorrectly deposited in the subcutaneous layer or within the muscle planes, which explains the less efficient anesthesia.10,11 Weintraud and colleagues12 have reported that diffusion of the local anesthesia solution occurred in the right plane only in 14% when the block was performed blindly. In this study also, we found a mean duration of analgesia of only 7 hours (vs 18 hours by USG) after blind TAP block. Ultrasound allows an increase in the duration of analgesia and a decrease in consumption of rescue analgesics in 24 hours as it is under real-time guidance which allows precise location of space and administration of the drug under vision with fewer complications.
In the current study, we found that the TDA was prolonged significantly in the USG group (18.88 ± 6.18 hours) as compared to the blind group (8.38 ± 2.58 hours) and total consumption of analgesics (TCA) were less in Group U (0.95 ± 0.67 g) than in Group A (2.54 ± 0.71 g). This result was very similar to Mankikar et al.8 who found that with USG-guided TAP block, the TDA was prolonged from 4.1 to 9.53 hours, and consumption of analgesia was also reduced in cesarean patients. In our study, we proved statistically that the total consumption of analgesics is less in exploration cases even after blind block. Hence, even blind block in the unavailability of USG machine is very useful for providing postoperative analgesia in patients with less dissection like exploration.
Recently, Aveline et al.13 have compared USG-guided vs blind TAP block in hernia patients. They found that patients who received USG-guided TAP block expressed significantly less pain at rest on VAS score at 4, 12, and 24 hours and postoperative morphine requirement was also less in the first 24 hours. Sunita et al.14 noted the time to rescue analgesia was more in the group who received USG-guided hernia block (7.22 hours) as compared to the group who received blind (6.80 hours) block.
In the current study, pain intensity at rest and movement was lower in ultrasound-guided TAP block. Pain score was further reduced in exploration cases of ovarian cystectomy and postpartum tubal ligation than in TAH which could be attributed to more amount of tissue dissection in TAH. Analgesic demand was decreased in patients who benefited from a USG-guided TAP block, as observed by the consumption in both the groups. Similar results were found by Petersen et al.15 in patients of laparoscopic cholecystectomy.
The most important benefit of giving TAP block, especially USG-guided, as part of multimodal analgesia for postoperative pain relief, is the total avoidance of opioids and a decreased consumption of other analgesics like NSAIDs, tramadol, and even paracetamol. All supplementary analgesics have side effects—nausea and vomiting being the common one, which decreases the postoperative satisfaction of the patient and also increases the postoperative stay. It is a very useful technique in patients with coagulopathy, poor cardiopulmonary reserve, and hemodynamically unstable patients. Local infiltration can also be given for postoperative pain relief but its action does not last long. The patient has more compliance with single-shot nerve blocks rather than giving multiple top-ups or using a patient controlled analgesia (PCA) pump with epidurals.
Transversus abdominis plane block has been associated with complications like local site infection, local anesthetic toxicity, peritoneal perforation, bowel injury, etc.16 No such complications were observed in our study except in one case where a rectus sheath hematoma was found, which was later found to be related to surgical complications.16 Blind TAP block has been documented with one case of liver puncture17 and colon injury has been observed after a blind inguinal block.18
Our study has several limitations. More number of patients need to be given USG-guided TAP block to get more appropriate results. Availability of the ultrasound machine by itself could be a problem in an institute other than a tertiary care center. Transversus abdominis plane block is limited only to somatic anesthesia of the abdominal wall; hence, newer techniques (like quadratus lumborum block variants) have been proposed to accomplish somatic as well as visceral analgesia. We did not include the type of incision, such as, transverse lower abdominal or vertical in our study. The point worth noting is that the vertical incision involves a greater number of dermatomes. We monitored VAS for pain score rating which is a subjective parameter.
CONCLUSION
This randomized single-blind study demonstrated that the USG-guided TAP block provides a longer duration of postoperative pain relief and reduced consumption of rescue analgesics till 24 hours as compared with conventional anatomical landmark-guided blind blocks after gynecological abdominal surgeries. Though TAP block can be safely given by conventional landmark-guided method, it provides the same degree of a duration of analgesia as USG-guided method only in minor cases that involve fewer dermatomes.
ACKNOWLEDGMENTS
The authors sincerely thank the Department of Anaesthesiology, Gynaecology and obstetrics Surgery and other staff of operation theater and administration of institution for permission to study and providing facility to carry out the work.
REFERENCES
1. Kehlet H, Wilmore DW. Evidence-based surgical care and the evolution of fast-track surgery. Ann Surg 2008;248(2):189–198. DOI: 10.1097/SLA.0b013e31817f2c1a.
2. Rawal N. Epidural technique for postoperative pain gold standard no more? Reg Anesth Pain Medicine 2012;37(3):310–317. DOI: 10.1097/AAP.0b013e31825735c6.
3. McDonnell JG, O’Donnell B, Curley G, et al. The analgesic efficacy of transversus abdominis plane block after abdominal surgery: a prospective randomized controlled trial. Anesth Analg 2007;104(1):193–197. DOI: 10.1213/01.ane.0000250223.49963.0f.
4. Carney J, McDonnell JG, Ochana A, et al. The transversus abdominis plane block provides effective postoperative analgesia in patients undergoing total abdominal hysterectomy. Anesth Analg 2008;107(6):2056–2060. DOI: 10.1213/ane.0b013e3181871313.
5. Atim A, Bilgin F, Kilickaya O, et al. The efficacy of ultrasound-guided transversus abdominis plane block in patients undergoing hysterectomy. Anaesth Intensive Care 2011;39(4):630–634. DOI: 10.1177/0310057X1103900415.
6. Rafi AN. Abdominal field block: a new approach via the lumbar triangle. Anaesthesia 2001;56(10):1024–1026. DOI: 10.1046/j.1365-2044.2001.02279-40.x.
7. Carney J, Finnerty O, Rauf J, et al. Studies on spread of local anesthetics: solution in TAP block. Anesthesia 2011;66(11):1023–1030. DOI: 10.1111/j.1365-2044.2011.06855.x.
8. Mankikar MG, Sardesai SP, Ghodki PS. Ultrasound-guided transversus abdominis plane block for postoperative analgesia in patients undergoing caesarean section. Indian J Anaesth 2016;60(4):253–257. DOI: 10.4103/0019-5049.179451.
9. Kaur M, Sahoo S, Vajifdar H, et al. Brachial plexus block: comparison of two different doses of clonidine added to bupivacaine. J Anaesthesiol Clin Pharmacol 2013;29(4):491–495. DOI: 10.4103/0970-9185.119147.
10. Yndgaard S, Holst P, Bjerre-Jepsen K, et al. Subcutaneously versus sub fascially administered lidocaine in pain treatment after inguinal herniotomy. Anesth Analg 1994;79:324–327.
11. Willschke H, Marhofer P, Bösenberg A, et al. Ultrasonography for ilioinguinal/iliohypogastric nerve blocks in children. Br J Anaesth 2005;95(2):226–230. DOI: 10.1093/bja/aei157.
12. Weintraud M, Marhofer P, Bösenberg A, et al. Ilioinguinal/iliohypogastric blocks in children: where do we administer the local anesthetic without direct visualization? Anesth Analg 2008;106(1):89–93. DOI: 10.1213/01.ane.0000287679.48530.5f.
13. Aveline C, Le Hetet H, Le Roux A, et al. Comparison between ultrasound-guided transversus abdominis plane and conventional ilioinguinal/iliohypogastric nerve blocks for day-case open inguinal hernia repair. Br J Anaesth 2011;106(3):380–386. DOI: 10.1093/bja/aeq363.
14. Khedkar S, Bhalerao P, Yemul-Golhar S, et al. Ultrasound-guided ilioinguinal and iliohypogastric nerve block, a comparison with the conventional technique: an observational study. Saudi J Anaesth 2015;9(3):293–297. DOI: 10.4103/1658-354X.154730.
15. Petersen PL, Stjernholm P, Kristiansen VB, et al. The beneficial effect of transversus abdominis plane block after laparoscopic cholecystectomy in day-case surgery: a randomized clinical trial. Anesth Analg 2012;115:527–533. DOI: 10.1213/ANE.0b013e318261f16e.
16. Jankovic Z, Ahmad N, Ravishankar N, et al. Transversus abdominis plane block: How safe is it? Anesth Analg 2008;107(5):1758–1759. DOI: 10.1213/ane.0b013e3181853619.
17. Farooq M, Carey M. A case of liver trauma with a blunt regional anesthesia needle while performing transversus abdominis plane block. Reg Anesth Pain Med 2008;33(3):274–275. DOI: 10.1097/00115550-200805000-00016.
18. Johr M, Sossai R. Colonic puncture during ilioinguinal nerve block in a child. Anesth Analg 1999;88(5):1051–1052. DOI: 10.1213/00000539-199905000-00015.
________________________
© The Author(s). 2021 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted use, distribution, and non-commercial reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.